Jacob Z. Hess, Ph.D.
Have we learned enough as parents to trust the Pfizer vaccine as effective and safe for young children over the long-term? In my own review, there are at least three important concerns that still need to be resolved.
Originally published on Meridian Magazine, November 5, 2021
After the data submitted by Pfizer for its COVID-19 vaccine for children received a thumbs up by the FDA panel last week, the anticipated nudging of parents began.
- Anthony Fauci said, “Even though the chances of (a child) getting sick and seriously ill are small, why do you want to take a chance of that with your child, when you can essentially protect the child by an intervention that is proven to be both highly effective and very safe?”
- Andrew Pavia from University of Utah Health likewise stated potential risks of the child vaccine are “dwarfed by the benefits of getting the vaccine.”
- Dean Blumberg, an associate professor of pediatric infection diseases at UC Davis concluded, “it’s clear the benefits outweigh the risks for this age group.”
- And Pfizer itself declared their vaccine offered children “a high degree of protective efficacy against COVID-19 during a period when the Delta variant of concern predominates in the US.”
Finally, after their own committee approved the shot’s distribution on Tuesday, CDC Director Dr. Rochelle Walensky suggested that “Parents should feel comforted not just that their children will be protected but that this vaccine has gone through the necessary and rigorous evaluation that ensures the vaccine is safe and highly effective.”
What more needs to be said? Seems like time to lay aside any further questions, and move on to getting shots in those trembling arms, right? (while anticipating additional data coming soon about children 5 and under).
I have learned over the last year that for many people, statements like those above are all the assurance they need. And I get it: ‘If a body of experts placed in positions of importance to evaluate the safety of medical interventions says something is safe, who are we to say otherwise?’ I really do understand – especially among a busy public weary and stretched thin after nearly a year and a half of roller-coaster pandemic. If a step like this could potentially help further normalize things in all the ways we keep hearing about (preventing more kids from getting sick, keeping schools open, contributing to herd immunity), why wouldn’t we be open to it – and even eager about it?
On this basis, the Biden administration has already purchased enough doses of Pfizer and Moderna’s vaccinations for up to 28 million children ages 5-12 years in the U.S. (with 109,000 pediatric doses of the vaccine pre-ordered and anticipated to show up in Utah by Tuesday, according to the Utah Department of Health).
But do we as parents really know enough to go along with this big step – and even support mandates that will likely emerge in many schools? In a Deseret News article entitled, “Should you vaccinate your 5-year-old,” Bethany Mandel emphasized her support for adult COVID-19 vaccination, before stating “if the government wants to mandate the COVID-19 vaccine for my kids…as many suspect they might after it’s approved, they need to make a much stronger public case that it’s necessary for kids as young as 5.”
When it comes to children with rapidly developing brains, it’s widely accepted that a more careful level of analysis needs to be brought to bear – even though that doesn’t always happen with pediatric studies.[1] Especially when it comes to our children, rather than taking others’ word for it (even important others), I would argue we need to be thinking for ourselves about whether or not the available evidence is strong enough for us to feel good about our children receiving it.
That’s our question to grapple over too. No, we’re not all “vaccine experts.” But we are parents. And our stewardship gives us a responsibility and an ability to discern for ourselves.
So, do you feel able to do that yet?
This isn’t an easy question – even when you’re hearing many statements like these above, and very little serious concerns expressed in prominent media outlets. Most of us have already heard the widely disseminated summary statement from Pfizer that the results are “91% effective against symptomatic infection” for children. You’ve also likely heard how the side effect profile was similar to older cohorts, with no serious adverse effects, how they created a smaller dose, etc.
But there are other parts of the study you likely haven’t heard about – but probably should. In what follows, I’m going to try and help you navigate the available data a little more – summarizing other details of the Pfizer study report referenced by the FDA and CDC to justify conclusions about safety and efficacy (including the FDA briefing document, and their original application here). None of what I’m about to say is hearsay or scandalous. It’s directly from the company’s own data.
This isn’t new territory for me. I’ve conducted a randomized controlled trial for youth before, and reviewed data from many other studies, especially those exploring pharmacological outcomes. My hope is this lay review will be especially helpful to other parents seeking to make these important decisions for their children.
Because of the hyperpolarized atmosphere all around us, I also feel compelled to add one thing more by way of preface: The vast majority of reporting on the Pfizer study and FDA proceedings involve a simple recapping of what government scientist have concluded (including those claiming to “break down the data”). To the degree that efforts like mine to provide additional scrutiny and critical evaluation of studies like this get automatically cast as forays into “dangerous misinformation,” or a signal that things are being “politicized,” what does that say about our ability as a public to ask our own serious questions, and to request more information from elected and public officials when necessary? If that ability goes away, it should be of concern to us all.[2]
But, I believe we can still do this! (Disagree, trust, deliberate, seek truth, stay united). Let’s think through this a little more together.
What does it take to demonstrate safety and effectiveness? Thoughtful experts still disagree on what it takes to ascertain conclusively that a newly developed vaccination for children is safe and effective against COVID-19. On one hand, you’ve heard the consistent answer from our national regulators: this study of a few thousand children is sufficient on both points. For many others, however, they’d like to see more. For these other experts (and parents), evidence that would pass muster would involve at the very least the following three conditions:
- A large enough sample size to be able to detect adverse effects that only show up in a smaller subset of cases
- A representative enough sample and analysis to be able to speak to real-world applicability of the vaccine and realistically evaluate the fully spectrum of possible benefits and risks.
- And enough time passing after the second dose to be able to confirm the treatment group of children is faring better long-term, while making sure we are also avoiding any of the more serious risks we’ve come to watch out for in other young people.
Those are not controversial or unrealistic standards – or at least they shouldn’t be. They’re reasonable to many scholars and parents generally. And yet, as you will see below, the data Pfizer submitted to regulators raise some fairly significant questions in each of these three areas:
1. Big enough. In a public statement earlier this fall reassuring parents that the FDA would “follow the science on COVID-19 vaccines for young children,” acting FDA Commissioner Janet Woodcock said, “because young children are still growing and developing, it’s critical that thorough and robust clinical trials of adequate size are completed to evaluate the safety and the immune response to a COVID-19 vaccine in this population.”
How well does this study meet that standard? Pfizer’s primary cohort involved 2,300 children (ages 7-12) and Modern’s study [with further details not yet released] involved 4,700 participants (ages 6-11). One of the most common concerns raised is that both samples are simply too small to detect an adverse effect such as myocarditis (which runs at a rate of around seven per million in adults). As reported by one epidemiologist observing the meetings, Pfizer also assessed the effectiveness of the vaccine-induced antibodies against the Delta variant using a subsample of only 34 children.
As Aaron Siri cautioned, “underpowered” studies like this will not “pick up anything but the most common adverse events.” He continues, “Without a clinical trial of sufficient size that reviews all potential adverse events, for a sufficient duration, [significant adverse effects] will not be identified prior to authorization or licensure.” This explains why international scientists proposed years ago that “inadequately powered studies should themselves be considered a breach of ethical standards.”
The final sample in this case was going to be even smaller, but to their credit, the FDA asked Pfizer to expand the trial earlier this summer. Instead of expanding that sample size, the company imported data from a second cohort (labeled as a “safety expansion” group) involving 2,379 participants followed for 2.5 weeks. The combined sample size was still small enough that, given the relatively low COVID-19 rates in children ages 5 to 11, there ended up being zero cases of severe COVID-19 and zero cases of death from COVID in either the treatment or control groups. As they describe the 19 total cases of sickness in the summary, “none of these cases met the criteria for severe COVID-19.”
This is important, as one analyst pointed out, so that you recognize this news about “91% protection” is referring (in this data) to protection against mild cases – cases from which, others note, children usually recover quickly, and with broad spectrum immunity.
Given how consistently these mild cases strengthen immunity, it’s fair to ask whether reducing them is even a desired clinical outcome. That’s perhaps what prompted Dr. Geert Vanden Bossche to raise concern about the potential of mass vaccination of the “young and healthy” potentially “erod[ing] their protective innate immunity towards Coronaviruses and other respiratory viruses.”[3]
Sidenote: How do you evaluate effectiveness without the presence of serious illness? Since there were zero severe cases of COVID-19 in the clinical trial, you can see that any direct analysis on that basis was disallowed. That creates quite a research challenge – and one that led to some interesting analyses. Instead of actual health outcomes, attention was turned to antibodies in a smaller sample of children; although generally speaking a poor predictor of immunity, these became the basis for this novel analysis.[4]
The Pfizer researchers summarize what happened next as follows: “Vaccine effectiveness was inferred by immunobridging SARS-CoV-2 50% neutralizing antibody titers.” Toby Rogers explained “immunobridging” like this:
Pfizer looked at the level of antibodies in the bloodwork of another study involving people 16 to 25 years old, they figured out the level of antibodies that seems to be protective in that population, then figured out how many kids ages 5 to 11 had similar levels of antibodies in their blood, and then came up with a number for how many cases, hospitalizations, ICU admissions, and deaths would be prevented by this shot in the 5 to 11 population in the future, based on the antibody levels and health outcomes from the 16 to 25 year old population.
Did you follow that? Based on these immunobridging estimates, researchers then performed another extrapolation – attempting a “quantitative benefit-risk analysis to evaluate predicted numbers of symptomatic COVID-19 cases, hospitalizations, ICU admissions, and deaths that would be prevented per million fully vaccinated children 5-11 years of age.” These are the numbers that have been widely shared as additional evidence for the need to take this step – for instance, claims that this additional wave of vaccination would lead to “approximately 600,000 fewer cases nationwide from November 2021 to March 2022” (along with emphasis on many associated benefits – more in-class teaching, more social interactions for children, less work interruption for parents, etc.).
This evaluation of antibodies was presented as the “primary analysis” – with the “secondary” analysis centering on evaluation of vaccine efficacy “against laboratory-confirmed symptomatic COVID-19 occurring from 7 days after Dose 2.” Because sheer observed cases were not sufficient to determine vaccine efficacy on their own, then, we’re relying on extrapolations and predictions to reach that conclusion.
Summing up, the Pfizer sample was too small both to detect adverse effects and evaluate preventive effects on any serious illness. That prompted an antibody analysis as another attempt to demonstrate effectiveness.
2. Representative enough. The well-known standard for research studies of any kind is a “representative” sample that reflects the diversity of the population to which results will potentially be applied. In actual practice, however, it’s common for clinical studies to screen and exclude people from research participation due to a variety of factors – always with a specific rationale for how it might interfere with the integrity of the research design. It’s also common for certain portions of the data to be excluded from the final data analysis, for various other reasons.
Both kinds of data restrictions happened in this particular study, which deserves attention to ensure the results are representative enough to all our children.
Sample limitations. The sample of children itself had some limitations evident from the beginning. For instance, as reported in the New York Times, Dr. James Hildreth criticized Pfizer “for including few minority participants in its clinical trial for 5- to 11-year-olds, saying that it could harm the confidence parents might have in the shot.”
During the study itself, other events influenced the characteristics of the final sample. For example: (a) Eleven children dropped out during the study, as they say, “mainly due to voluntary withdrawal.” (b) 10 children in the treatment group were excluded from the results for “protocol deviations” compared to 0 excluded from the placebo group (see note number 17 at the bottom for more on why this may matter). And (c) by the end of the study, nearly 5% of participating children did not report final numbers – as they note: “Among Cohort 1 participants, 95.1% had safety follow-up ≥ 2 months after Dose 2 at the time of the September 6, 2021 data cutoff.”
What happened to those other 4.9% children without any reported safety follow-ups after dose 2? Were they in the vaccine or placebo groups? No further information is given about those specific youth – and in a sample this small, it’s not hard to imagine the combination of these exclusions and drop-outs could sway results in different directions.
Analytic limitations. Clearly, the study did include children across most relevant backgrounds (prior COVID-19 infection or not, immunocompromised or not). But it’s worth noting that based on publicly available reports, the formal analyses on which decisive calculations were based did not appear to include children with prior COVID-19 infections.[5] As one reporter summarized FDA meeting over the results, “The risk/benefit analysis also did not take into account natural immunity protection.”
So, what can we say about study participants 5-11 years of age without evidence of prior COVID-19 infection? Not much. The summary does seem to point towards this as a future analysis with results to be released one day.[6] Yet when it comes to results presented as evidence to make this decision, it seems clear that both main analyses were based on a “population of participants without evidence of prior SARS-CoV-2 infection” (page 18).
This detail does not show up in popular reports on the study, however – which mostly repeated the various summary statements.[7] Yet this seems a nuance important enough not to overlook. With an estimated 42% of kids with natural protection against COVID-19, why would they leave kids like that out of the critical final analysis? As noted earlier, controlling for (or screening out) anything that might influence or “contaminate” results is a common practice in controlled trials. And given how much naturally acquired immunity appears to exert a significant protective effect, it makes some sense why some might be curious about evaluating the vaccine’s effect purely on children without infection-derived immunity.
Yet skeptics are quick to highlight this as one reliable way to make study results look especially good – since you’re essentially eliminating a factor that could likely dilute the positive treatment effect. The question still remains: What can be said from these results about children with natural immunity? Would the vaccine make any difference for these children? (This was raised by one FDA panel member – wondering whether the vaccine would “help that much” the 42% of children with natural immunity). We might also wonder, does the shot impact natural immunity in any way – for better or worse?[8]
Once again, there’s no way to tell from the analyses presented, given their focus on those without prior infection. Yet of course, children of all different backgrounds will be included in the likely vaccine roll-out – and would all be subject to any mandate that is instituted, such as in California schools.[9]
Similar concerns showed up even among advisory board members at the FDA. As Katelyn Jetelina reported from the meeting, “Two members voiced frustration that this was a binary choice: all or nothing vaccine for 5-11 year old’s. Some asked whether they could rephrase the question for specific kids, like obese or immunocompromised.” It’s precisely these individual complexities that prompts mothers like Bethany Mandel to argue that “Each scenario should be analyzed independently and parents should be given the space to make personal calculations without fear of mandate or undue pressure.”
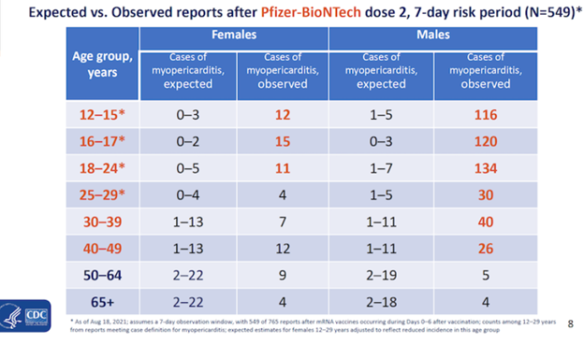
It has surprised some that the risk-benefit models created by the FDA look exclusively at only one known harm from previous COVID-19 vaccination of children — myocarditis. That specific analysis of myocarditis has prompted a number of questions among observers as well.[10] How serious is this specific risk? On one hand, some researchers have argued that vaccine-induced myocarditis is a “much more mild form of disease” –insisting on its rarity and showcasing the likelihood of recovery. By comparison, others insist “myocarditis is not a mild side-effect. It’s dead muscle in the heart.” As Neil Oliver puts it, “You can’t have ‘mild myocarditis’ – in the same way you can’t be ‘a little bit pregnant.’”
What would the actual numbers of myocarditis in children be if we proceeded with a national vaccination campaign for this age group? The FDA estimates that there will be 106 extra myocarditis cases per 1 million fully vaccinated children 5-11. With 28,384,878 children ages 5 to 11 in the U.S, that would translate into 3,009 excess myocarditis cases post-vaccination if all children received it.
Although healing and recovery are still clearly possible for many affected youth, those estimates again vary widely. On one hand, the CDC committee claimed 83% of affected children in available data had fully normal cardiograms three months later – with one epidemologist calling it a “rare side effect…reported among 397 adolescents…of which, the majority were mild and resolved within days.” Others point with concern towards the aggregated rates of myocarditis in youth tracking to date,[11] alongside estimates of a 20% fatality rate after 2 years and a 50% fatality rate after 5 years for myocarditis.
Bottom line: Many believe this is a serious and demonstrable risk we would be accepting if we moved forward – based on a dataset that, as noted above, was unable to make any direct observations about reductions in serious illness or death. This explains why Utah scientist, Dr. Brian Dressen, appearing before the FDA panel before its decision last week, testified: “Each of you hold a significant responsibility today and know that without a doubt, when you approve this for the 5-11-year-old’s, you are signing innocent kids and uninformed parents to a fate that will undoubtedly rob some of them of their life.”
This man wasn’t a “conspiracy theorist.” He was a researcher simply wanting to encourage the panel to consider an expanded study that would “decisively demonstrate that the benefits outweigh the risks for children.” Dressen went on to catalog some of the same issues reviewed above: expressing concern that the “decision is being rushed, based on incomplete data from underpowered trials, [and] insufficient to predict rates of severe and long-lasting adverse reactions.”
Which brings us to the final, critical question.
3. Long-term enough. Exactly how long is needed to legitimately determine safety and effectiveness in any treatment evaluation study? That’s a question I’ve spent much of my career exploring – writing about it recently at length in anticipation of this FDA decision (see Long-term, Short-term). In this Pfizer study, the first cohort has been followed for 2 months to assess adverse effects, with the second cohort followed for 17 days. It should hardly need pointing out that 2 months isn’t sufficient to assess the full spectrum of longer-term risks, let alone 2.5 weeks.
More time is needed for careful follow-up. Although the FDA’s own planned follow-up typically extends to 6 months after the 2nd dose, unfortunately more rigorous follow-up (in comparison to a control group) won’t likely happen with these children, since those who initially received the placebo will get vaccinated at the end of the study – as Pfizer researchers say, for “ethical reasons.”
But what about the ethics of rigorously tracking controlled data over time – and having some solid, longer-term reassurance of what we’re prescribing widely?[12]
This is especially important considering how quickly we’re learning the situation changes in the weeks and months following COVID-19 vaccination for adults. And Robert Malone points out these shots will “likely have to be repeated twice for each school year” (at approximately six month intervals) – it won’t be a “one-and-done.” As data analyst Mahesh Shenai notes, “due to their youth,” these younger groups of children are especially “vulnerable to the unknown risks realized in the future.”
Any more serious analysis of long-term effects is proposed by Pfizer researchers as a future study if they turn up.[13] That explains why Dr. Eric Ruben justified his “yes” vote on the FDA panel by saying, “We’re never gonna learn about how safe the vaccine is until we start giving it. That’s the way it goes.”
Suffice it to say, given the decisions of our regulatory bodies this week, we don’t (and won’t) know much more about how the vaccine affects a child long-term – at least until it’s actually administered to many children.
Competing evaluations of overall cost-benefit. Some might read all of this and wonder, ‘why not wait to do a little more research before moving forward, like so many others have proposed? Is that really such an unreasonable proposition to make?’
Others will say, ‘okay, so there are issues with the study. But aren’t there concerns with every study? Should we be so ‘picky’ when there’s an emergency happening?’ The latter is more of what we are hearing in national media – with a central focus on how threatening COVID-19 is for children. As Dr. Andrew Pavia at University of Utah Health was quoted as saying, “Children are really suffering from COVID-19 – children 5 to 10 can get really sick with COVID.” The analysts involved in this FDA approval likewise noted that as of Oct. 21, nearly 6.3 million children have tested positive for COVID-19 since the onset of the pandemic.
What receives significantly less attention in national media outlets is that since the beginning of the pandemic 50,000 U.S. children under the age of 18 have died from other causes – yet the CDC noted this summer 335 documented deaths in children due to COVID-19. That’s why the American Academy of Pediatrics stated just last month: “At this time, it appears that severe illness due to COVID-19 is uncommon among children.”
Certain children are clearly more vulnerable than others. And a recent CDC analysis likewise confirmed that children who died from COVID-19 tended to be older than 10 and had at least one underlying medical condition. According to a 2021 Johns Hopkins study of about 48,000 children under 18 years old diagnosed with Covid, the mortality rate was zero in children without a pre-existing medical condition such as leukemia. As Bethany Mandel summarized in the Deseret News, “Yes, children can get sick and can even die from COVID-19. But, statistically speaking, the risk for children under 10 of developing major complications from COVID-19 is really low. It’s close to nothing.”[14]
Although the FDA and CDC reviews of Pfizer data acknowledge some of this, they only touch on it, before redirecting attention to the threat of COVID-19 for children and others around them. That makes sense, given how much this disease has impacted us all – and will likely continue to do so. I’m thinking especially of parents of immunocompromised children like our own daughter. How should we balance some of the (still) unknown risks of vaccination with the possible consequences of COVID-19 for the more vulnerable children? (MIS-C, long-COVID, or myocarditis itself).
None of this is easy to navigate, and can be so confusing. But I am comforted in knowing that God is not confused, and surely can provide personalized guidance to help each of us in making the best decisions for our families and individual children. Of course, these calculations ought to go beyond the well-being of children alone, to seriously consider the best ways to protect vulnerable adults as well. The precise impact of vaccination in this equation long-term continues to be debated, since COVID-19 vaccines have not protected against transmission as much as people once hoped. In this case, as one epidemiologist pointed out, “Pfizer did not assess asymptomatic disease (and thus transmission) in the clinical trials” for children. But it’s still worth thinking about carefully.
But when it comes to the health of children alone, it’s not entirely clear to some that there is a health crisis to address. As Saul Faust, a professor of pediatric immunology and infectious disease, argued recently, “On balance, there is no urgency to immunize children from a medical perspective.” And analyst Toby Rogers went so far as to suggest that there was “no emergency in this population for which one could apply for Emergency Use Authorization.”
At the very least, it does seem there is more to talk about. Indeed, some of these numbers start to suggest a very different cost-benefit ratio. Asserting that “the vaccine has saved lives and has been an absolute medical miracle for those most at risk,” Bethany Mandel said, “we’re getting into a new stage of a vaccination campaign, one where the cost-benefit analysis is more complicated.” She then proposed that “Above all, parents need to be able to trust that the powers that be approving these vaccines are deliberating as seriously as they would were they making medical decisions about their own children.” Noting the “bullying and condescension that has marked the campaign to vaccinate the reluctant among us adults up to this point,” Mandel goes on to insist parents of young children deserve better – even “a frank accounting of the risks of the vaccine and of the virus for their children.”
What will your own evaluation be? As you can see, these differing appraisals of the overall circumstance lead to very different risk/benefit ratios. We already cited earlier Dr. Pavia’s feeling that risks from this vaccine were “dwarfed by the benefits of getting the vaccine.” Andy Larsen concluded in the Salt Lake Tribune that the available data reviewed by public health benefits “outweighed the public health costs by a substantial margin” – adding, “it wasn’t a close call, as the margins between the pros and the cons were even larger than most pediatric vaccines approved.” Dr. Fauci’s own estimation of this child vaccine as now “proven to be both highly effective and very safe” prompted his question, “Even though the chances of (a child) getting sick and seriously ill are small, why do you want to take a chance of that with your child.”
Others might wonder in reverse, ‘Even though the chance of a serious adverse effect from the vaccine may be small, why would you want to take a chance of that with your child?’ In this camp is Robert Malone, who had a hand in developing mRNA technology, concluding that this data confirms there is “minimal if any direct clinical benefit to the child” and shows it “will not prevent infection.” Given the likelihood of continued dosage every six months, he continues: “the risk of adverse events such as cardiomyopathy will be cumulative. Each shot will be another roll of the dice.”[15]
Referring to this risk, one parent whose daughter almost died from myocarditis said, “Why would I take the chance of another child of mine having myocarditis over the chance of a mild illness from Covid? Why would anyone?”
So, once more: is it a “roll of the dice” to have your child get the shot – or not get it? That depends on the expert you trust, and ultimately on your own discernment as a parent.
To conclude, I can’t help but ask: if you were sitting on the FDA panel yourself, given all the above, would you agree that this preventive treatment meets these four established criteria for issuing an Emergency Use Authorization?
- “The [threat] can cause a serious or life-threatening disease or condition.”
- “Based on the totality of scientific evidence available, including data from adequate and well controlled trials, if available, it is reasonable to believe that the product may be effective to prevent, diagnose, or treat such serious or life-threatening disease or condition that can be caused by SARS-CoV-2.”
- “The known and potential benefits of the product, when used to diagnose, prevent, or treat the identified serious or life-threatening disease or condition, outweigh the known and potential risks of the product.”
- “There is no adequate, approved, and available alternative to the product for diagnosing,
preventing, or treating the disease or condition.”
What would you decide? What will you decide for your own family?
My own conclusion. After reviewing doing this deep dive myself, here are my thoughts. Millions of children from all backgrounds and risk categories are going to be vaccinated in the weeks and months ahead based on a study design and analysis that is too small and too short-term to detect any serious risks. In taking this step, we will also be relying on analyses focused on the subset of children without natural immunity and relying on extrapolated cases based on estimates from antibodies.
By comparison, what would happen in a study that analyzes all the complexities of adverse effects and backgrounds in a sample ten times as big – and with a 6-month follow-up?
Would we be reaching the same conclusions? And making the same choices?
I can’t imagine we would. I’ve tried not to be skeptical of motives here – and to assume the best intentions.[16] But sometimes it’s okay to allow yourself to consider a more skeptical, and critical vantage point. In this case, I would say: Do you want to make your results in a pharmaceutical outcome study look as good as possible? Then implement as many of the following steps as possible:
1. Make your cut-off (for both primary efficacy analysis and adverse effect tracking) short enough that you don’t have to deal with the messy complexities (decreasing immunity, increasing side effects) that inevitably arise later on.
2. Make your sample size small enough that you have less likelihood of detecting the kinds of more serious adverse effects that inevitably emerge in the larger population.
3. Keep your sample “clean” by getting rid of anyone that violates protocol[17] – and then pursue the “cleanest” analysis of cases that show the most “helpful” results.
4. If adverse effects do arise, propose further review and analysis – and reassure the public that until that happens, they cannot be definitely linked to the vaccine.[18]
I am not suggesting that Pfizer researchers consciously designed the study in this way. But as someone that has conducted research for years, I know well the strong incentives that exist in all organizations to design a study that will be most helpful to your overall mission. So, no, you don’t have to be skeptical of motives to have serious questions. Many of the research patterns I’ve raised questions about are norms in pharmaceutical research – and continue a line of investigation I’ve pursued for years now.[19]
May Higher wisdom guide us all in our own families and stewardships. But whatever we end up deciding, let’s dispense with the idea that the available evidence will cleanly answer the question for us. As you can see above, the available data is hardly up to the task.
Note: Special thanks to analyst Toby Rogers and others for work on which this draws – attempting here to summarize it for a popular audience. I’ve been fascinated by competing narratives of health, illness and treatment for nearly two decades – starting with my dissertation work around competing narratives of Prozac and depression. Since then, I’ve published peer-reviewed analyses of competing interpretations of the mentally ill brain, the process of recovery from severe mental illness, and what it means for a child intervention to be “effective.” The bulk of my pandemic writing has focused on deepening empathy and understanding across competing narratives of appropriate COVID-19 response – including a new two-part picture book that attempts to visualize some of the greatest contrasts involved in the escalating conflict, entitled “The Special Shot That Saved (and Divided) the World.”
Notes:
[1] As I’ve demonstrated with data from youth-prescribed antidepressants and how youth evaluation studies are often designed.
[2] By many measures, we’ve already arrived at a very concerning place. Listen carefully to how this New York Times reporter characterized the surprising number of concerning messages sent to the regulatory bodies by parents and others in this approval process: “Before they met, advisers to the F.D.A. and the C.D.C. were bombarded by thousands of emails offering misinformation about the vaccine and asking the experts to vote against it.” Were any of the concerns being raised worth considering? Apparently not. After all, they were simply “misinformation.”
[3] Speaking of these children, Bossche continued:
Their innate immunity normally / naturally largely protects them and provides a kind of herd immunity in that it dilutes infectious Coronavirus pressure at the level of the population…Children/ youngsters who get the disease mostly develop mild to moderate disease and as a result continue to contribute to herd immunity by developing broad and long-lived immunity.
[4] To their credit, they acknowledge the tenuous scientific backing of what they’ve done on the bottom of page 15: “No specific neutralizing antibody titer has been established to predict protection against COVID-19…The immune marker(s) used for immunobridging do not need to be scientifically established to predict protection but should be clinically relevant to the disease.”
[5] Read for yourself from the FDA Briefing document about the Pfizer results, where it states:
- On page 24: “In participants 5-11 years of age without evidence of SARS-CoV-2 infection prior to Dose 2, the observed vaccine efficacy (VE) against confirmed COVID-19 occurring at least 7 days after Dose 2 was 90.7%, with 3 COVID-19 cases in the BNT162b2 group compared to 16 in the placebo group. All cases of COVID-19 occurred in children without prior history of infection. None of these cases met the criteria for severe infection. Comorbidities at baseline (including obesity) were present in total of 20.1% of cases.”
- On page 32: “Vaccine Efficacy (VE) against symptomatic COVID-19 after 7 days post Dose 2 up to October 8, 2021 (data cutoff) was 90.7% in participants 5-11 years of age without evidence of prior SARS-CoV-2 infection. Totals of 3 cases of COVID-19 occurred in the BNT162b2 group and 16 in the placebo group, most of which occurred during July-August 2021 when the Delta variant was prevalent in the United States. At the time of the data cutoff, none of these cases met the criteria for severe COVID-19.”
[6] From page 17: “Phase 2/3 is being conducted in the United States, Finland, Poland, and Spain…[and] did not exclude children with a history of prior SARS-CoV-2 infection or clinical symptoms/signs of COVID-19.”
[7] For instance, one article said, “three vaccinated children caught covid, while there were 16 cases among the placebo group—almost 91% effectiveness.”
[8] A salient question with the more complicated longer-term picture now emerging for adults.
[9] With 1.8 million documented infections in the 5-11 year old age group, and with 1 in 4.2 infections reported, up to 8 million children may have had asymptomatic exposure – so this is a significant group of children. As one analyst summarizes “What is the expected benefit of vaccination to this group, and is it outweighed by the risks?”
[10] One analyst summarized the concerns:
[Pfizer] estimate “excess” myocarditis (caused by the shot) using data from the private “Optum health claim database” instead of the public VAERS system (p. 32) – which makes it impossible for the public to verify their claims. Then, when it comes to estimating how many children with vaccine-induced myocarditis will be hospitalized and admitted to the ICU they use the Vaccine Safety Datalink (see page 33). Why switch to a different database for those estimates? Finally, there is no explanation for how they calculated “excess” myocarditis deaths, so they just put 0.
[11] For instance:
[12] Whether or not it’s the right thing to wipe out a control group like this (or to stop tracking negative outcomes long-term at all), both are common practices in pharmacological outcome studies (as they acknowledge on page 8, “Deaths are recorded to the end of the study”).
[13] As they say on the bottom of page 16, “Post-licensure/post-authorization safety surveillance and observational studies in pediatric populations would be needed to evaluate for adverse reactions that occur too rarely to be detected in clinical trials.”
[14] The data really does back this up strongly. In a meta-analysis combining data from 11 countries, Stanford researchers Cathrine Axfors and John Ioannidis found a median infection fatality rate of 0.0027% in children ages 0-19 – with a 99.9973% survival rate among infected children. And among 45 states reporting mortality, children were 0.00%-0.26% of all COVID-19 deaths, with seven states reporting zero child deaths. Data also confirms that in states reporting, 0.00%-0.03% of all child COVID-19 cases resulted in death.
[15] When it comes to teenage vaccinations, by the way, many of the same study limitations above were involved in the data submitted to regulators for their authorization – leading some to similarly wonder if those initial studies would adequately capture actual risk. Subsequent analyses of real-life adverse effects among teenagers, including one recent review by researchers at the University of Southern California, found that rates of myocarditis for healthy teenage boys after two shots of Pfizer/BioNTech vaccine were up to four times more frequent (94-162 cases per million, depending on age) compared with healthy teens getting hospitalized for COVID-19 (44 per million).
[16] That’s always the best and most Christian way to proceed. I gave the same benefit of the doubt to critics of the Church of Jesus Christ in their widely publicized studies “showing” damning things about our faith (see John Dehlin analysis here and Jana Riess analysis here).
[17] If a child is injured after the first dose, they were dropped from the trial. As one commentator added, “The rules of the trial were that all recipients experiencing side effects were to have them addressed by a study doctor. Seeking medical care outside of the study automatically results in the subject’s removal from the study. Since severe side effects are likely to result in an emergency room visit at the local hospital, this ensures the majority of serious side effects will be parsed from the study data.”
[18] Which, of course, is often true – including of the four identified on page four: “4 participants reported serious adverse events; all were considered by the study investigator and FDA as unrelated to vaccination.” Yet there are other instances where even devastating cases from the teen trial have continued to be widely denied as having any connection – with the CDC insisting that zero deaths connected to myocarditis among youth could be confirmed due to the vaccine.
[19] Ten years ago, Florida State University professor Jeffrey Lacasse and I made similar observations about psychiatric trials happening for children. After reviewing the same kinds of analytic issues (short vs. long-term, etc.), we concluded that peer-reviewed analysis saying:
In the absence of attention to these kinds of questions, we submit that researchers may, even unaware, set up studies that are predisposed toward positive results—for example, short-term investigations using surface-level measures that minimize both participant voices and negative outcomes. Ensuing results may then be presented to potential clients and the broader public as evidence that X therapy or Y medication works.

Well done Jacob. There is no reason for children to take these vaccines, unless they are in the very small group of people who are at extremely high risk from COVID, and this group is less than 1 percent of children worldwide. COVID is not a threat to children, but the vaccine is. Check out this FDA presentation in which the FDA admits that under some scenarios the RISK OF THE VACCINE IS HIGHER THAN THE VIRUS. It is unbelievable but true. Read it yourself:
https://www.fda.gov/media/153507/download
I’m so grateful for the well-researched and thoughtful perspective Jacob Hess has contributed to this topic during a season of craziness and confusion. What a blessing! Thank you.
Here’s the covid experience in my close family when we all got it at the same time:
Unvaccinated unhealthy grandma – admitted to ICU given antibodies, ivs, etc.
Vaccinated unhealthy grandpa- refused admission or not tested, because he’s vaccinated (early days, when docs were in denial), in equal bad shape. Eventually they gave test, was positive. Both recovered. Grandpa has had some reoccurrences of covid like sickness though.
1yr old – no symptoms
Nursing mother, flu symptoms, rough but functional.
9yr old – no symptoms
11 year old – no symptoms
13 year old – cold symptoms, sniffy, drippy nose.
15 year old – cold symptoms, same
Me – slightly sore, one night of cold sweats, mild occasional cough, continued vigorous exercise throughout.
That experience seems to match the general population trends based on age/health. Sorry Fauci it’s no real risk to my family. The vaccine is unknown though. Thanks but no thanks for your concern.
Thanks for this analysis. I work in the pharmaceutical field, but not in Drug Product, in which this gene therapy jab is associated. I’m also not a bio or pharmacology specialist. But I still get questions from many people. I have been advising everyone who has asked, and my entire family, that they should not have this shot administered to any children (18 and under) unless that child has severe health issues that are likely to result in severe reaction to the Covid infection. The World Health Organization still has the official position that, since children almost never have any significant symptoms, and almost none who don’t have other huge health issues have died, there is no justification for subjecting them to higher risk by administering the so-call vaccine.
I am appalled that the CDC, the FDA and the manufacturers have by-passed all the protocols that have been required for many decades for a drug to be approved. I was able to accept “emergency authorization” for adults, especially those in high risk situations. The rest is just plain irresponsible. I can only assume the following: some have great delusions of power and are now addicted to that; some feel compelled to take this position in order to maintain their positions and jobs (giving in to peer pressure); or greed for the money involved. Remember that reportedly 20 to 25% of medical professionals have not received the jab. Most of those will be or are already out of a job because of their own ethics.
If anyone, as a parent, has even an inkling that perhaps his or her child should be administered this vaccine, please fast and pray after as much study of the test results (not just what is touted by the FDA, CDC, and medical establishment).
Good comment cheute79
This is a very useful review of the issues inherent in the approval process. Thank you Brother Hess for the work that went into producing this analysis.
Given what was presented in this post (and it seems to have been done in a fairly even handed manner) I would agree the studies were too small, and the time periods involved too short. Additional clinical studies seem to be justified/needed.
I think one point the government administrators and the companies seem to be avoiding is that the main benefit to be derived from vaccinating millions of children is the herd immunity aspect of the process. It needs to be well proven that we wouldn’t be putting those millions of children at an unnecessary level of risk to obtain that benefit – I agree the submitted studies are not rigorous enough to prove that no significant harm is being done.
Brother Hess, keep up the good work!